Neuropathy is a complication that is bothersome and not very often addressed or treated properly. This complication gradually develops over a period of time and is

Cause of type 1 diabetes: Type 1 Diabetes is due to an absence of insulin secretion by the pancreas from birth. Most of the cases of

Though close to 85% use the internet even if from the low socioeconomic population, digital technology and web based application usage has been very slow to catch

Smoking has been the passion of many though the prevalence has come down from a lofty 40% in 1965 to 20.9% in 2006. 90 %

Normally during the cold winter months, the levels of HbA1C, the 3 month average of sugar, can be higher due to higher food quantity consumed to

Glycemic index ( GI )of a food is the increase in blood glucose ( above fasting glucose) 2 hours after ingestion of a constant amount of food
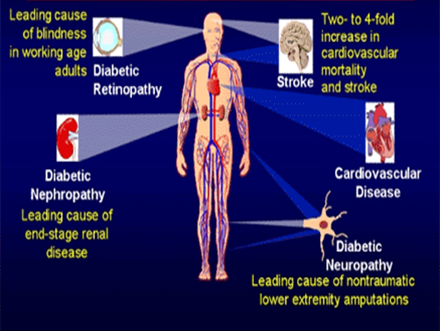
Did you know that every ten seconds a person dies from diabetes related complications? Diabetes is the fourth leading cause of global death by any disease.
This is a state of disillusion, frustration and a meek submission to diabetes which results in complete disregard to blood sugar level management. This is regarded as
Once we are born, we all have to die someday. During the course of our life, we learn a lot from our experiences, sometimes we do not.

In todays world,one needs to relax in