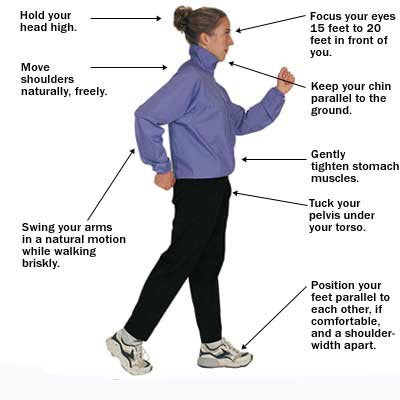
From time immemorial, man has been walking for traveling to reach one place, to hunt and gather food for self and family and also in search of

Cause of type 1 diabetes: Type 1 Diabetes is due to an absence of insulin secretion by the pancreas from birth. Most of the cases of
This presentation discusses the problems associated with this special population, what exercises can be done and what medicines can be taken safely.

This is one area many are still unsure of. It is generally assumed cutting down the carbohydrate intake to as low as possible when one is a
Fasting from dawn to dusk in the holy month of Ramadan for healthy adult Muslims has been ordained and physically sick Muslims are exempt from it.

Though close to 85% use the internet even if from the low socioeconomic population, digital technology and web based application usage has been very slow to catch
Once we are born, we all have to die someday. During the course of our life, we learn a lot from our experiences, sometimes we do not.

Indications for insulin usage: When oral medicines fail to control the sugar in maximum doses when there are complications to the eyes, kidney or heart, when

Driving regulations vary from country to country. But, the fitness to drive especially if one is a diabetic is the same around the world . Driving
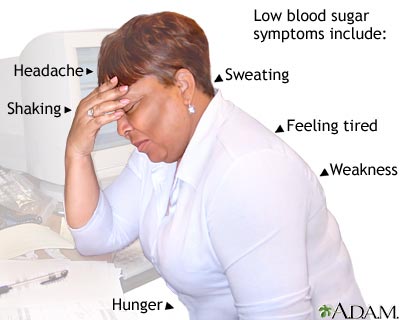
Hypoglycemia or low sugar is one of the nightmares of the patients and the doctors alike. High and low sugars may both present with sweating ,