Though close to 85% use the internet even if from the low socioeconomic population, digital technology and web based application usage has been very slow to catch

Smoking has been the passion of many though the prevalence has come down from a lofty 40% in 1965 to 20.9% in 2006. 90 %

Normally during the cold winter months, the levels of HbA1C, the 3 month average of sugar, can be higher due to higher food quantity consumed to

Though essential, there are many bad effects with salt when taken in large amounts over a long period of time. The kidneys cannot get rid of this
This is a state of disillusion, frustration and a meek submission to diabetes which results in complete disregard to blood sugar level management. This is regarded as

In todays world,one needs to relax in

Summer is here again. Here, in the Middle east, there are just 2 seasons, summer and a cool season ( not exactly winter). The months

Indications for insulin usage: When oral medicines fail to control the sugar in maximum doses when there are complications to the eyes, kidney or heart, when
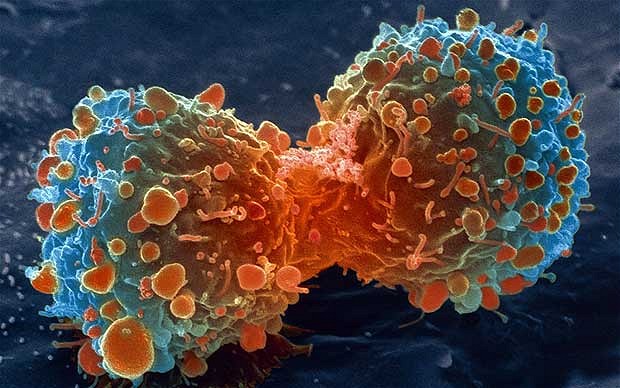
Cancer care for women Cancer is one major problem these days and it has become so common to hear of someone known to you, perhaps, on treatment

Driving regulations vary from country to country. But, the fitness to drive especially if one is a diabetic is the same around the world . Driving