It is known the Fasting happens during the month of Ramadan during the day light hours. Different parts of the world have different timings for fasting due
Lot of money has been pumped in the research to make the management of diabetes less painful and better to help in better compliance of medications. All

There are many types of insulin each working in its own unique manner, some types of insulin are suitable for one but not for another. Normally basal

New insulin delivery devices . LifeScan One Touch Via® This is a super slim pump device which delivers only bolus (rapid acting ) insulin. The cartridge can
Fasting from dawn to dusk in the holy month of Ramadan for healthy adult Muslims has been ordained and physically sick Muslims are exempt from it.

Glycemic index ( GI )of a food is the increase in blood glucose ( above fasting glucose) 2 hours after ingestion of a constant amount of food
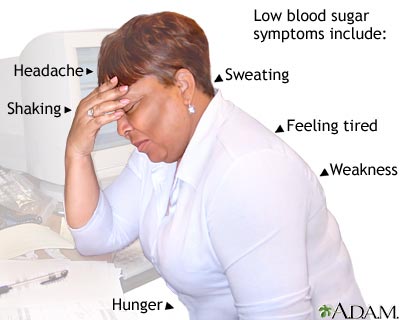
Hypoglycemia or low sugar is one of the nightmares of the patients and the doctors alike. High and low sugars may both present with sweating ,

If you have diabetes, one needs a blood glucose meter — a small device — to measure, store and display the blood glucose level. Glucometer is