Though essential, there are many bad effects with salt when taken in large amounts over a long period of time. The kidneys cannot get rid of this

Glycemic index ( GI )of a food is the increase in blood glucose ( above fasting glucose) 2 hours after ingestion of a constant amount of food
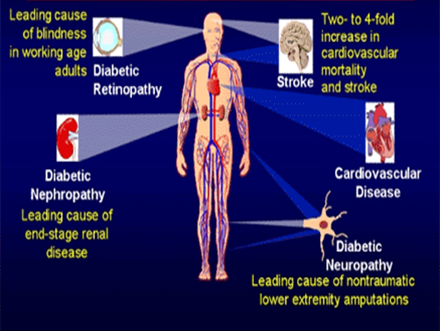
Did you know that every ten seconds a person dies from diabetes related complications? Diabetes is the fourth leading cause of global death by any disease.

Bariatric surgery is known to be the most effective and long lasting treatment for morbid obesity and many related conditions, but now mounting evidence suggests it may
This is a state of disillusion, frustration and a meek submission to diabetes which results in complete disregard to blood sugar level management. This is regarded as
Once we are born, we all have to die someday. During the course of our life, we learn a lot from our experiences, sometimes we do not.

In todays world,one needs to relax in

Weight loss Sometimes despite the intense effort and hard work put in, the weight loss is not as expected . One also tends to notice that a

Summer is here again. Here, in the Middle east, there are just 2 seasons, summer and a cool season ( not exactly winter). The months

Dietary Cholesterol is seen in all animal products such as meats, dairy products and eggs, deep fried items, processed food and some of the bakery products