This is a state of disillusion, frustration and a meek submission to diabetes which results in complete disregard to blood sugar level management. This is regarded as

Dietary Cholesterol is seen in all animal products such as meats, dairy products and eggs, deep fried items, processed food and some of the bakery products

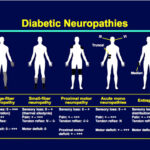
Indications for insulin usage: When oral medicines fail to control the sugar in maximum doses when there are complications to the eyes, kidney or heart, when
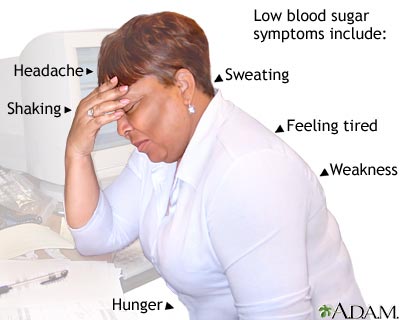
Hypoglycemia or low sugar is one of the nightmares of the patients and the doctors alike. High and low sugars may both present with sweating ,

If you have diabetes, one needs a blood glucose meter — a small device — to measure, store and display the blood glucose level. Glucometer is